Horticultural Therapy in Patients with Stroke: Three Case Series
Article information
Abstract
Horticultural therapy (HT) is the engagement of a person in gardening related indoor activities by a trained professional to achieve specific treatment goals. It was effective as an alternative medicine and played an important role in rehabilitation of stroke patients, especially in psychological aspects. While the psychological benefit has been clearly demonstrated, the evidence of the physical benefit is insufficient. We report three stroke patients treated with HT and they were evaluated from the standpoint of physical, psychological, and cognitive outcomes. HT program consisted of 10 sessions during 2 weeks with 1 hour per session. The assessment of outcomes and positron emission tomography/computed tomography (PET/CT) were performed before and after treatment. Two patients showed improvements in physical and psychological aspects. But the other patient showed no outstanding outcome. These results suggest the possibility of HT as a complement to conventional occupational therapy.
Ⅰ. Introduction
Horticultural therapy (HT), a nature-assisted therapy involves plants, natural materials and outdoor environments to hasten recovery and rehabilitate patients (Annerstedt and Wahrborg, 2011). Some of the effects of HT are found to be disorders in terms of psychological matter (Kim et al., 2003;Soderback et al., 2004;Annerstedt and Wahrborg, 2011;Kamioka et al., 2014). HT was suspected to be effective for mental and behavioral disorders such as dementia, schizophrenia, depression and terminal care for cancer in 4 randomized controlled trials, although quality of studies was low (Kamioka et al., 2014). It also increased social participation, health, well-being and life satisfaction for patients with brain damage (Soderback et al., 2004). HT was tried as an alternative medicines in Korea to relieve neuropsychological symptoms in a small group of stroke patients (Kim et al., 2003).
Scientific evidence of HT for the functional improvements in stroke is insufficient (Soderback et al., 2004; Kim et al., 2003). However horticultural therapists are brought up in 25 universities nationwide, and are certified biannually. The Korean Ministry of Rural Development and Administration even introduces the applications of the horticultural therapy to be the rehabilitation for persons with disabilities. Further study is needed to verify whether HT has other effects other than from psychological aspects, and whether it could be incorporated into comprehensive rehabilitation therapies.
We report three stroke patients treated with HT and evaluated with physical, psychological, cognitive outcome measures, and 2-deoxy-2-[18F] fluoro-D-glucose positron emission tomography- computed tomography (PET/CT) before and after HT.
Ⅱ. Materials and methods
1. Horticultural therapy
HT was applied to three stroke patients who were admitted to Dankook University Hospital. All patients had mobility impairment because of muscle weakness by stroke, so HT was performed not to outside but in hospital. All patients received HT in the same occupational therapy room at the same time. We carried out therapy at 6 p.m. from December 18 to 30, 2014. The HT program included 10 one-hour sessions for two weeks, which consisted of 1-to-1 therapy by a horticultural therapist (Table 1). The activities of HT was selected by the reports (Kim et al., 2010).
2. Cognitive outcome measure
The Korean version of Mini-mental State Examination (K-MMSE) is a brief 30 point questionnaire test that is used to screen for cognitive impairment and composed of 8 categories: orientation to time, orientation to place, registration, attention and calculation, recall, language, repetition, complex commands.
3. Physical outcome measure
The Rapid Upper Limb Assessment (RULA) is a simple scale initially developed to evaluate the ergonomic risk factors associated with musculoskeletal disorders. It is divided into the following body regions: upper and lower arms, wrist, neck, trunk, and legs and higher scores correponding to increased range of motion and muscle power (McAtamney and Corlett, 1993). The RULA was once reported to be used as an evaluation tool for stroke (Jeong et al., 2015).
The Korean Version Modified Barthel Index (K-MBI) is an ordinal scale used to measure performance in activities of daily living. It consists of 10 items: personal hygiene, bathing, eating, toileting, stair climbing, dressing, bowel control, bladder control, ambulation or wheelchair, chair-bed transfer.
4. Psychological outcome measure
The Korean version of WHO Quality of Life scale (WHOQOL) is a self-reporting multidimensional measure which is composed of the important aspects of life and covers not only physical health status but the psychological, social and spiritural domains of life. It contains six domains: physical domain, psychological domain, levels of independence, social relationship, environment domain, spiritual domain.
The geriatric Depression Scale Short Form-Korea version (GDSSF-K) used to identify depression in the elderly. It is a subset of 15 questions with the highest correlation with depressive symptoms.
5. Radiologic outcome measure
PET/CT is a imaging test that allows to see how brain is functioning. It captures images of the activity of the brain after radioactive tracers have been absorbed into the bloodstream. These traces are attached to compounds like glucose. Active area of the brain will be utilizing glucose at higher rate than inactive areas and It is highlighted under a PET scanner.
Ⅲ. Results
1. Case 1
A 52-year-old man with alleged hypertension developed a left posterior inferior cerebellar arterial infarction and was transferred to the rehabilitation unit on 37 days after stroke. His main complaint was ataxia, with the Berg balance scale 17/56, and the Korean version of Modified Barthel Index (K-MBI) 59/100.
The HT was started on 58 days after stroke, in combination of conventional physical therapy and occupational therapy after informed consent. The patient showed profound interest, concentration, and satisfaction in HT from the first day of treatment and improved interpersonal competence among other patients from the 3rd day. Patient-therapist interaction was enhanced from the 5th day and maintained until the end of the sessions.
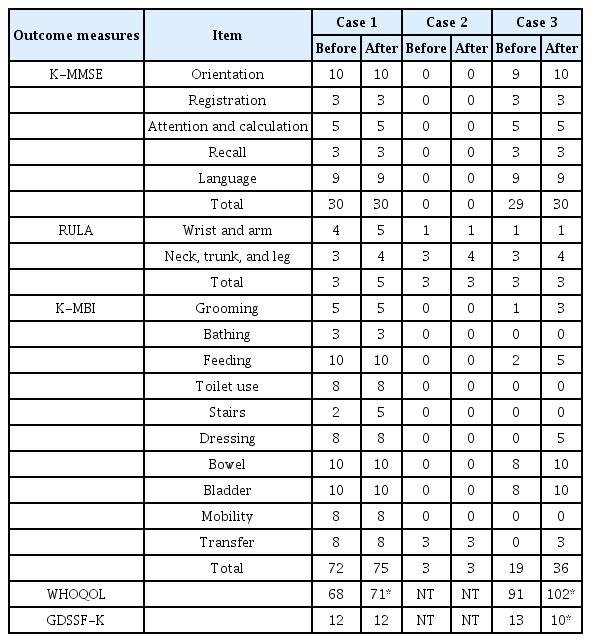
All the outcome measures were evaluated before and after HT: K-MMSE, RULA, K-MBI, WHOQOL, and GDSSF-K The K-MBI (only the stair domain), WHOQOL, and RULA (all domains) scores were improved after treatment (Table 2). The second FDG PET/CT showed suspicious FDG uptake decrease in bilateral cerebral hemispheres, but it was thought to be an artifact (Fig. 1A, 1B).

(A) FDG PET/CT before treatment in case 1. FDG uptake was decreased in the left posterior cerebellum. (B) FDG PET/CT of case 1 showed a reduced FDG uptake in bilateral cerebral hemisphere after treatment. (C) FDG uptake was moderate severely decreased around left parietal lobe, cingulate gyrus, basal ganglia and thalamus in FDG PET/CT of case 2 before treatment. (D) In the second FDG PET/CT of case 2, FDG uptake along right cerebral hemisphere and left cerebellum was increased.
2. Case 2
A 57-year-old man with a left middle cerebral arterial infarction was referred to the rehabilitation unit on 31 days following stroke. Main problems were right hemiparesis (muscle strength was grade 0/5), global aphasia, severe cognitive impairment (K-MMSE 0/30). Conventional physical therapy and occupational therapy were performed for these problems.
While neurologic and functional recoveries were slow, he gradually became depressed over 126 days after onset, the symptom was diagnosed as a major depressive disorder and prescribed antidepressants. The HT was started at the particular time. The program and outcome measurements were the same as the Case 1. The patient was nervous, non-participative, and getting tired at first, but then on the 4th day of HT, he showed interest, positive attitude and tried to participate in HT. As the cooperation with the therapist got better, the reactions and expressions about the HT activities increased from 8th day. The WHOQOL and GDSSF-K were not testable due to severe cognitive impairment. The K-MMSE, K-MBI, and RULA did not show differences before and after treatments (Table 2). Neck/trunk/leg score on RULA was improved 4/5 from 3/5, but total score did not change (Table 2). In the second FDG PET/CT, FDG uptake(mainly temporal area and left cerebellum) along the right cerebral hemisphere increased (Fig. 1C, 1D). The reason seemed to be due to diaschisis effect.
3. Case 3
A 35-year-old pregnant woman without any underlying disease developed a spontaneous intracerebral hemorrhage in the right basal ganglia, and transferred on 24 days after stroke. The patient had left hemiparesis (muscle strength grade 0-1/5). The K-MBI score was 19/100 and K-MMSE score was 29/30.
HT was started on 26 days after stroke with conventional physical therapy and occupational therapy. She had become to be and active participant in treatment and showed improvement of communication and interpersonal competence skills with each HT. The WHOQOL score increased while the GDSSF-K score decreased after treatment. There were also increments in some domains of the K-MBI and RULA, but total RULA score did not changed (Table 2). FDG PET/CT was not performed because of pregnancy.
Ⅳ. Discussion
Three cases of stroke patients treated with HT were informed above. This might be the first time to apply HT as a part of conventional occupational therapy to subacute stroke patients in Korea. The increase in WHOQOL in case 1 was larger than the minimal clinically important difference (MCID) of WHOQOL, which is 1 (Den Oudstein et al., 2013). The increment in the K-MBI might have occured due to conventional physical therapy rather than HT because the only change was in stair score. Both wrist/arm score and neck/trunk/leg score were improved in the RULA. No definite changes were observed in case 2. It may be due to the fact that this case has severe cognitive, language, and motor impairment initially. The K-MBI and WHOQOL in case 3 rose to the extents greater than MCID (15 in the K-MBI (De Morton et al., 2011), and 1 in WHOQOL) after HT.
The RULA was used in these case studies because other upper limb assessments tools require instruments and longer period, and are sometimes difficult to test lower function. Even though, the RULA may need more detailed validation in subacute stroke patients.
FDG PET/CT, instead of functional magnetic resonance imaging (fMRI), was performed to demonstrate brain activities due to hospital’s limited resources. The fMRI with better temporal and spatial resolution might have reveal definitive changes in brain.
In addition to psychological benefits, HT might improve physical functions. RCTs including larger population should be performed in near future to elucidate the neurologic and functional effects of HT in stroke. Before proceeding to a planned RCT, this case series are meaningful as a test of feasibility of HT and RULA in each stroke patient with different lesion and severity.
References
Annerstedt, M. and P. Wahrborg. 2011. Nature-assistedtherapy : Systemic review of controlled and observational studies. Scand. J. Public. Health. 39:371-388.
De Morton, N.A., N.K. Brusco, L. Wood, K. Lawler, and N.F. Taylor. 2011. The de Morton Mobility index (DEMMI) provides a valid method for measure and monitoring the mobility of paitents making the transition from hospital to the community: an observational study. J. of physiothe. 57:109-16.
Den Oudstein, B,L,, W,P, Zijlstra, and J, De Vries. 2013. The minimal clinical important difference in the World Health Organization Quality of Life instrument-100. Support. Care. Cancer. 21: 1295-301.
Jeong, C.P., D.H. Shin, T.S. Park, J.H. Choi, J.I. Moon, and S.H. Yang.2015. Study of Adjusted Rapid Upper Limb Assessment for evaluating of rehabilitation effects, Key. Eng. Mater. 625:644-48.
Kamioka, H., K. Tsutani, M. Yamada, H. Park, H. Okuizumi, and T. Honda. 2014. Effectiveness of horticultural therapy : A systemic review of randomized controlled trials. Complement. Ther. Med. 22:930-43.
Kim, M.Y., Kim, G.S., Mattson, N.S., and Kim, W.S. 2010. Effects of horticultural occupational therapy on the physical and psychological rehabilitation of patients with hemiplegia after stroke. 28:884-90.
Kim, S.Y., K.C. Son, H.J. Jung, J.H. Yoo, B.S. Kim, and S.W. Park. 2003. Effect of horticultural therapy on functional rehabilitation in hemiplegic patients after stroke. J. Kor. Soc. Hort. Sci. 10:780-85.
McAtamney, L. and N. Corlett. 1993. RULA : A survey method for the investigation of work-related upper limb disorders. Appl. Ergon. 24:91-9.
Soderback, I., M. Soderstrom, and E. Schalander. 2004. Horticultural therapy : The ‘Healing garden’ and gardening in rehabilitation measures at Danderyd Hospital Rehabilitation Clinic, Sweden. Pediatr. Rehabil. 7:245-60.